Consultant Recommends Substantial Hikes To RI DD Rates; Public Comment Invited
/By Gina Macris
The average pay of a direct care worker serving Rhode Islanders with developmental disabilities would jump almost four dollars to $22.14 an hour July 1 in a new rate structure recommended by a healthcare consultant to the state Department of Behavioral Healthcare, Developmental Disabilities, and Hospitals (BHDDH).
The proposed rate structure would make Rhode Island’s direct care workers the highest paid of any developmental disabilities caregivers in 26 states, according to the consultant, the Burns & Associates division of Health Management Associates.
Photo HMA-Burns
Stephen Pawlowski, an HMA-Burns official, presented the preliminary recommendations in video meetings Sept. 28 and Sept. 29. HMA-Burns and BHDDDH will accept public comment until Oct. 24 before finalizing the recommendations.
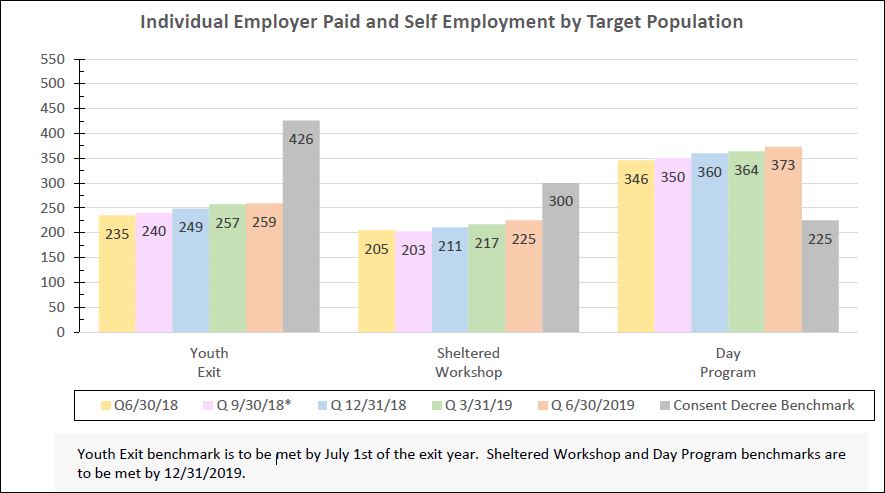
In compliance with a federal court order, the state has agreed to pay direct care workers a minimum of $20 an hour by 2024. To follow the state fiscal year, which begins in July, the new rate would become effective six months earlier than the court deadline. The $20 minimum means the average hourly pay will be $22.14, Pawlowski said. (see graphic, above)
Preliminary recommendations of the HMA-Burns also include significant increases in many other rates as part of a continued fee-for-service reimbursement structure for private service providers that has been in place for more than a decade.
Service providers, consumers and their families, and even a legislative commission have called for alternatives to fee-for-service reimbursements during the last several years.
Three dozen private agencies form the backbone of Rhode Island’s developmental disabilities system. The state relies on them to meet the requirements of a 2014 civil rights agreement mandating a network of individualized community-based daytime services by June 30, 2024 in accordance with the Integration Mandate of the Americans With Disabilities Act (ADA).
DELAY IN PART OF RATE REVIEW
A federal judge set a Dec. 1 deadline for completion of the rate review, but Pawlowski said the portion that deals with individual assessments and individual budgeting cannot be finished until mid-2023.
In August, an independent court monitor said this portion of the rate review should be completed by Oct. 31, underlining his recommendation in bold type in a report to the court.
The process and timeline involving assessments, service plans and developing individual budgets is “one of the most critical aspects of the transition to high quality person-centered practice,“ but the way these elements connect with each other is ‘‘poorly understood,‘‘ said the monitor, A. Anthony Antosh.
‘‘Person-centered practice‘‘ refers to a professional approach that that puts a client’s needs and preferences first in keeping with with the consent decree and the ADA.
Antosh recommended the state do a “comprehensive review“ of its use of the current assessment tool, the Supports Intensity Scale (SIS), citing continued problems with inaccuracies in the results.
The state made it clear a year ago that it will continue using the SIS, but during the recent presentations, the HMA-Burns spokesman , Pawlowski, that the publisher is in the process of revising it.
The second edition of the SIS is expected in January, 2023, he said. It will be incorporated into the new rate structure by mid-year, he said. The graphic below lays out additional details.
REVENUE HIKE FOR PROVIDERS
Overall, the various rate increases would hike revenues for private service providers 20 to 25 percent above current levels, Pawlowski said.
Part of the increase in private agency revenues would come from funding employment-related services, more costly than other types of daytime supports, as a separate add-on allocation.
It remains unclear how much one-on-one time with a direct care worker an individual would get under the proposed new rate model. One-on-one staffing is considered important for community integration.
Pawlowski was asked whether someone choosing one-on-one staff time exclusively would use up their budget allocation faster than someone in a small group. The short answer is “yes,” he said.
Anne LeClerc, a BHDDH official, added quickly that “it depends” on a person’s need and funding level.
On an hourly basis, the rate for one-on-one supports in the community would increase from $37.88 to $65. Not everyone will have a budget big enough to pay for one-on -one staffing for an extended period of time.
One caveat is that one-on-one staffing will be available to all who seek competitive employment in the community, regardless of the size of their individual budgets, BHDDH spokesman said.
Final answers to questions about the availability of one-on-one staffing will be directly linked to the way the new SIS version defines individual need and the funding that results from that definition.
The new system also includes a range of reimbursement rates for group supports in the community involving no more than three people for each worker.
Center-based care will continue, with its own range of reimbursement rates. Centers would be used as gathering places in the morning to prepare for community activities and places for daytime meals and personal care, Pawlowski said.
15-MINUTE BILLING UNITS
During the presentations, Pawlowski said new rate structure will continue 15 minute billing units for daytime services, giving consumers the “flexibility” to “mix and match” their choice of services and service providers.
Private agency providers for years have complained that the administrative cost and time used to bill in 15-minute increments according to staffing ratios detracts from their ability to provide the services themselves.
In one of many court-ordered activities, a cross-section of state officials and community representatives has studied 15-minute billing and found it burdensome, recommending that the 15-minute unit be replaced with one or two rates for community staffing lasting three or four hours at a time.
Pawlowski said the new model would reduce the administrative burden by eliminating the requirement to account for staffing ratios within each 15-minute billing unit.
Reimbursement tables in the proposed rate structure assume there will be five levels of funding, as there are now.
The funding levels are largely based on a person’s perceived ability or inability to complete the tasks of daily living, with the “tiers” of funding running from A, the lowest funding, to E, the highest.
“SELF-DIRECTED” CONSUMERS
About a quarter of consumers receiving developmental disabilities services do not rely on private agencies but direct their own plans, mostly with help from their families.
They are responsible for hiring direct care staff, but a fiscal intermediary handles payroll and helps them stay on track with their budgets.
Going forward, Pawlowski said, fiscal intermediaries will be limited to payroll services.
Support activities will become part of case management - a service now under review for all health and human service departments governed by the Executive Office of Health and Human Services to ensure that Rhode Island complies with federal case management rules.
The removal of support services from the role of the fiscal intermediaries will result in a slight rate decrease, Pawlowski said.
But some fiscal intermediaries listening to the presentation online said the two functions can’t be easily separated.
RESIDENTIAL OPTIONS TO WIDEN
Reimbursement rates would increase substantially for residential services except for the largest group homes, with six or more residents, where the rate reviewers assumed an economy of scale, Pawlowski said.
A few of the largest group homes would see a slight decline in funding, he said.
Rates for shared living, which Pawlowski said have remained the same since the program started, will get substantial increases. Shared living providers host adults with developmental disabilities in their homes.
For the first time, there will be an enhanced reimbursement rate for hosts who also provide all the day services for the people in their homes.
Established provider agencies that now oversee individual shared living arrangements will be required to make monthly visits to each home, Pawlowski said.
There are two new categories of residential services:
Supervised living, a shared service for those who don’t need 24-hour care and live near each other, like residents with separate apartments in the same building who are visited by the same “floating” staffer as needed.
Room and board arrangements in which an individual with intellectual and developmental disabilities has a roommate who is not the homeowner.
The proposed reimbursement scale also provides for “remote services” in which a worker can check in electronically and follow-up with an in-person visit if needed.
Recordings of two presentations and a packet of information on the proposed rates and other related materials have been posted to the BHDDH website at https://bhddh.ri.gov/developmental-disabilities/initiatives/rate-and-payment-methodology-review-project/public-review
Written comment from the public will be accepted until Oct. 24 at bsmith@healthmanagement.com
Graphics by HMA-Burns