Bill Promoting Olmstead Plan Passes RI Senate
/By Gina Macris
The Rhode Island Senate on May 21 passed a bill that would lead to an Olmstead plan for funding an array of community-based health and human services to prevent the unnecessary segregation of children and adults with disabilities.
The bill is moving through the General Assembly at a critical time, just a week after U.S. Attorney Zachary A. Cunha alleged the state has failed “miserably and repeatedly” to meet its legal obligations to provide appropriate services to children with mental health and developmental disabilities in their communities.
Instead, children and adolescents have been “warehoused” at the state’s only children’s psychiatric hospital, Bradley Hospital in East Providence, Cunha said, calling the state’s reliance on a single option an “appalling failure.”
The state must respond by tomorrow, May 23, to alleged violations of the Integration Mandate of the Americans with Disabilities Act (ADA), according to a spokesman for Cunha.
The Senate’s proposed Olmstead plan takes its name from a 1999 U.S. Supreme Court decision which reinforced the Integration Mandate of the ADA. The decision said the ADA requires public services for people with disabilities to be offered in the least restrictive environment that is therapeutically appropriate, and that environment is presumed to be the community.
Rhode Island is the only state in New England and one of seven in the nation that does not have an Olmstead plan, said Sen. Louis DiPalma, D-Middletown, in describing the bill on the floor of the Senate.
Last week’s allegations of civil rights violations serve as a prime example of the reason the state needs such a plan, said DiPalma, the chief sponsor of the legislation.
The bill, which has been sent to the House, would establish a 25-member commission to make annual recommendations for “integration for all” to the governor and the General Assembly, beginning on Jan. 15, 2025. The bill also requires the commission to do a comprehensive assessment of needs and accomplishments every five years.
More immediately, a spokeswoman for Governor Dan McKee has said the state will cooperate with the DOJ to resolve the brand new Olmstead civil rights allegations.
The findings, the result of a joint investigation of the U.S. Attorney’s Office and the Department of Health and Human Services, make two broad recommendations:
· The state must ensure that existing community-based services are available in sufficient quantity to prevent long and repeated hospitalizations at Bradley. These services include intensive in-home and community services, crisis services, and therapeutic foster care.
· The state Department of Children, Youth, and Families must make improvements in discharge planning to smooth the way for a prompt transition to the most integrated setting that is appropriate.
Rhode Island has a new law that could go a long way toward adequately funding community-based children’s services and satisfying the demands of the Olmstead complaint.
In 2022, the General Assembly enacted a requirement that all federal-state Medicaid reimbursement rates for struggling community-based social and human services undergo a review every two years by the Office of the Health Insurance Commissioner (OHIC).
The first OHIC rate review recommended hefty hikes which would have cost an estimated $90 million in state revenue in a single year, according to a spokeswoman for Governor McKee.
That does not include more than $50 million for health care providers outside the OHIC review and $29.1 million for Certified Community Behavioral Health Clinics, she said.
The governor has recommended implementing the recommended OHIC rates over three years, including $22.1 million that would represent the state’s share of the federal-state Medicaid match in the next fiscal year. He would also slow the pace of future rate reviews in each of four categories of services to once every four years.
But companion bills sponsored by DiPalma and Rep. Tina Spears, (D-Charlestown, South Kingstown, New Shoreham, and Westerly,) in the House would require the governor to use figures from OHIC rate recommendations in his budget. It would also require the twice-yearly caseload estimating conference to adopt the latest OHIC rate recommendations in advising the governor and the General Assembly on Medicaid costs for the next budget year.
In an email to supporters, Spears says those two bills “gained traction” after 100 advocates went to the State House May 14.
Grass roots advocacy for those relying on a broad array of community-based health and human services has been a hard slog for nearly 15 years.
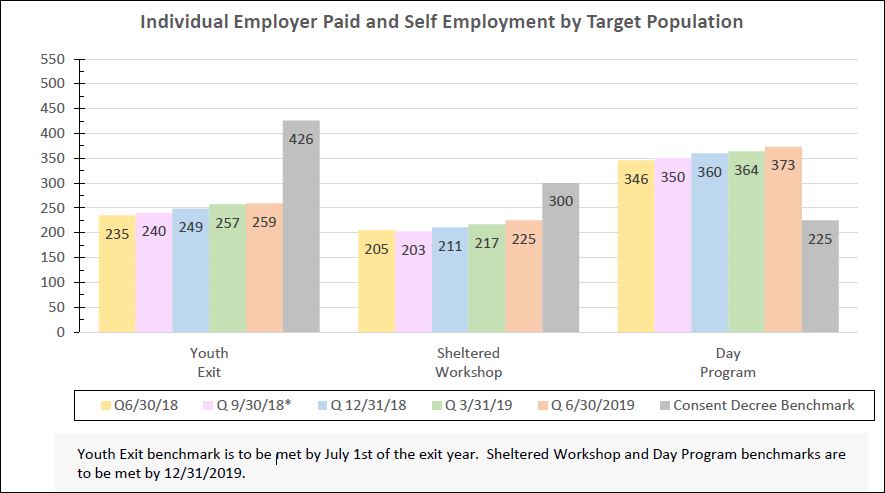
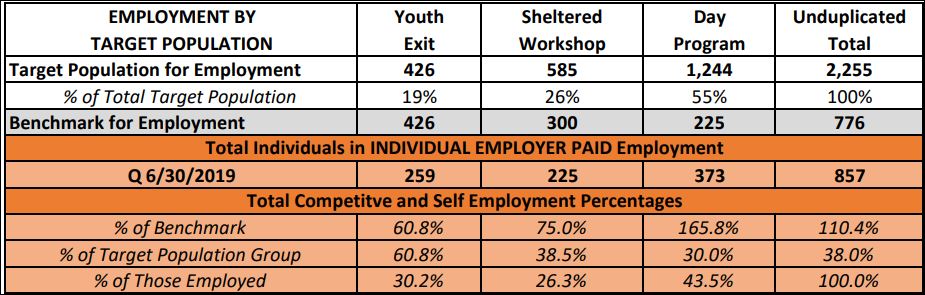
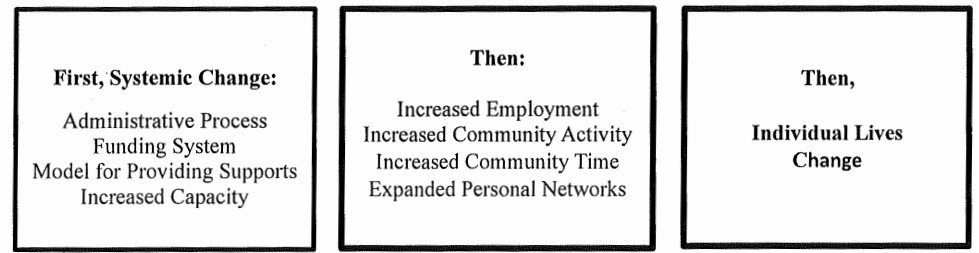
In 2014, the state entered into an Olmstead consent decree with the DOJ to end the segregation of adults with developmental disabilities. It was not until 2021, when it faced the threat of heavy fines for alleged non-compliance, that the state began overhauling Medicaid rates to community service providers and changing its approach to services for adults with developmental disabilities.
Those changes are still underway, and federal oversight continues in the developmental disabilities case.