RI Faces High Cost For Fixing DD ADA Violations
/By Gina Macris
After funding services for adults with developmental disabilities below their actual costs for nearly a decade, the state of Rhode Island is about to experience sticker shock.
The system of private agencies that provides most services for adults with developmental disabilities is on the verge of collapse, by all accounts, and a federal judge has given the state until Dec. 18 – five days from now – to come up with the money to keep it afloat until the next fiscal year.
The state also is under court order to devise and execute a plan for strengthening the system during the next three years so it can comply with a federal civil rights agreement that requires Rhode Island to integrate adults with developmental disabilities into community life by 2024. With the judge ready to use his power to enforce the consent decree, those costs could increase spending on developmental disability services by a third or more in the next several years.
Last month, a federal court monitor addressed the short-term fiscal gap by suggesting that the state release $2 million a month in unspent funds already allocated to developmental disabilities simply to keep the agencies’ doors open over the next six months. The COVID-19 pandemic has forced agencies to shrink services and drastically reduce billing.
Judge John J. McConnell, Jr.
In a recent hearing before Chief Judge John J. McConnell, Jr. of the U.S. District Court, a spokeswoman for service providers took a different approach, saying the state needs to immediately raise direct care pay, now an average of $13.08 an hour, to enable the private agencies to recruit and retain employees during the pandemic.
Roughly two thirds of these essential workers are women and more than half are people of color, according to the trade association spokeswoman.
A recently-completed report from the association, the Community Provider Network of Rhode Island (CPNRI), fleshes out projected costs:
An hourly increase of $2.32, to $15.50, would require nearly $44.1 million a year, or 16.4 percent more than the state has currently budgeted.
A hike to $17.50 would mean an additional $79.8 million, or a 29.7 percent increase in the annual budget
A $20 hourly rate would add $124.5 million to the budget. That would amount to a 46.4 percent increase in spending.
The report, “A System in Crisis,” said employers need to be able to offer $17.50 immediately to get job applicants in the door during the pandemic. In Fiscal 2022, which begins July 1, the rate should be increased again to $20 an hour.
Monitor’s Calculations More Limited In Scope
The monitor, meanwhile, agrees with the need for pay hikes, although he would allow the state more leeway on the timeline. In his latest report, filed with Judge McConnell Nov. 30, the monitor, A. Anthony Antosh, said the state should raise hourly wages to $17.50 “as quickly as possible” and to $20 by Fiscal 2024, which begins July 1, 2023.
A. Anthony Antosh
Antosh’s fiscal analysis focuses primarily on the changes needed in the final three years of the consent decree. He said there is consensus among various stakeholders with whom he has consulted that staffing and fiscal issues are the two main concerns in implementing the 2014 civil rights agreement.
“The state budget deficit resulting from the COVID-19 pandemic significantly complicates any fiscal analysis and any decision-making about budget planning,” he said.
Antosh makes no specific dollar recommendations but says that figures should be negotiated with provider agencies in a three-year budget plan to be completed in time to begin in the next fiscal cycle on July 1, 2021. He emphasized that the agencies provide 83 percent of the services necessary to support those protected by the consent decree.
Antosh said an ongoing review of the entire fiscal and reimbursement system, itemized in a 16-point court order issued by McConnell July 30, should be complete by June 30, 2021.
He also recommended that steps be taken now to make sure that the specific costs of a strengthened developmental disability system are acknowledged when future state budgets are being developed.
For example, the data on caseloads provided monthly by the Department of Behavioral Healthcare, Developmental Disabilities and Hospitals (BHDDH) to the General Assembly should be included in the Caseload Estimating Conference used to determine human service needs in the overall state budget. That is also one of the final recommendations of the “Project Sustainability Commission,” a a special legislative commission headed by Staite Sen. Louis DiPalma, D-Middletown.
While not acknowledging the actual costs, which pay for entitlement services under provisions of the Americans With Disabilities Act, the General Assembly has often criticized the state’s developmental disabilities system for running over budget.
The governor typically relies on the November caseload and revenue estimating conferences to draw up the budget that is submitted to the General Assembly in January. The legislature, in turn, relies on more finely tuned caseload and revenue estimates in May to finalize a spending plan for the next fiscal year.
Monitor’s Numbers “Illustrate” Solutions
Antosh’s report includes five sets of fiscal projections that can best be described as starting points for discussion rather than cost estimates for system-wide change. For reasons related to the language of the consent decree, the monitor’s numbers cover individuals who were identified in confidential documents between 2013 and 2016 and today make up about 67 percent of the entire population with developmental disabilities.
Antosh said the tables of projections and descriptions of the associated costs “illustrate” various options in reconfiguring daytime services for the 67 percent.
The most comprehensive “illustration “ of the cost of re-inventing daytime employment and leisure activities for the specific portion of the population protected by the consent decree would add $35.6 million to the budget in Fiscal Year 2022, which begins next July 1, Antosh said. An additional $14.9 million would be needed in Fiscal 2023 and $15.8 million extra would be added in Fiscal Year 2024.
In addition to protecting a particular class of people, the consent decree is supposed to lead to a system-wide transformation. And state officials have made clear that they intend to include all people eligible for developmental disability services in a reformed system, not just those identified at the time of the consent decree.
The three increases projected by Antosh add up to about $66.3 million a year in three years’ time. Antosh said the increases need not all come from Medicaid funding but draw on a variety of other public and private sources.
The current annual approved budget for the private service providers is about $268.7 million in federal-state Medicaid funds, although the providers’ ability to bill for reimbursement has shrunk since the start of the pandemic.
Actual spending on privately-run services was about $240.8 million in the fiscal year that ended June 30, 2019, according to state budget figures. Antosh said the increases need not all come from Medicaid funding but draw on a variety of other public and private sources.
CPNRI, meanwhile, offered estimates for system-wide reform that would not only increase wages but provide for more labor-intensive supports in the community in keeping with the requirements of the consent decree. The organization’s report said that at a direct care rate of $17.50 an hour, the more labor-intensive option would cost between $112.9 and $158.9 million, depending on the number of hours provided and other variables, including the level of independence of each individual as perceived by the state’s assessment tool.
CPNRI’s report incorporated work completed earlier this year by BHDDH consultants, as well as earlier projections done for the state by different consultants.
COVID-19 Exacerbates Inequities
The pandemic has highlighted the inadequacy of the poverty-level pay of direct care workers in the private sector. The average wage of $13.18 an hour falls below many entry-level jobs in retail, delivery, warehouse, restaurant and janitorial fields, according to the recent report from CPNRI.
That rate is also nearly $5 less than the $18 minimum hourly rate the state pays its own employees to do the same work, running a small parallel system of group homes for about 125 adults with developmental disabilities.
The years-long difficulties faced by providers in recruiting staff have reached critical proportions during the COVID-19 pandemic, leaving many individuals without services and crippling the agencies’ ability to generate income.
The crisis has been nine years in the making.
In 2011, the General Assembly devalued the private provider system when it adopted a new reimbursement model and budget cuts that were justified with an executive branch memo that simply said providers could deliver the same services with less money.
The $26- million budget cut resulted in layoffs and slashed wages. Entry-level positions for caregivers, once the starting point of a career ladder for caregivers who did not necessarily have college degrees, became minimum-wage, dead-end jobs.
At the time, the Department of Behavioral Healthcare, Developmental Disabilities (BHDDH) ignored the recommendation of an outside consultant who said direct care workers should receive a minimum of $15 an hour within a year’s time.
The state pleaded poverty in the aftermath of the financial crash of 2008 and 2009, but by 2011, most other states were either holding steady on previous cuts or beginning to reverse reductions in human service spending, including those for people with developmental disabilities.
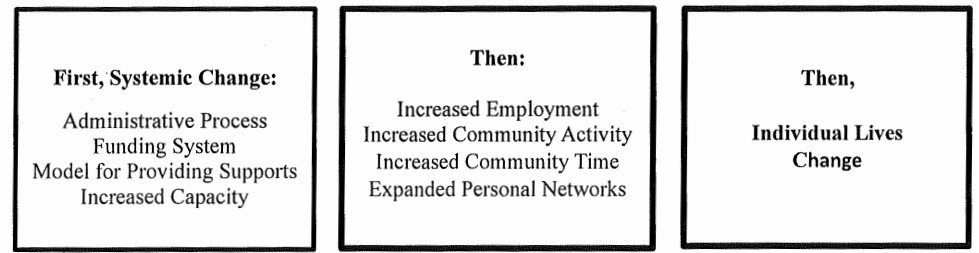
The austerity move accompanied a new reimbursement system billed as “Project Sustainability,” intended to equitably distribute available funds to eligible adults with developmental disabilities. The reimbursement model incentivized congregate care in sheltered workshops and day care centers – the least costly form of supervision. Subsequently, the DOJ found that an over-reliance on congregate care violated the Integration Mandate of the Americans With Disabilities Act. That finding led to the consent decree.
In a recent report, CPNRI said that COVID -19 has thrust a system developed and funded for congregate care into one that must deliver personalized services to mitigate infection among a vulnerable population.
Long-term effects of neglect on the system prevent providers from being “agile and responsive to meet the demand and needs of the community,” said the report. For example, the reimbursement model assumes that 40 percent of services will be delivered in center-based care, which is prohibited by public health concerns.
Read the court monitor’s report here.
Read the CPNRI report, “System in Crisis” here.