By Gina Macris
This article was updated June 17 with a response from the Rhode Island Department of Behavioral Healthcare, Developmental Disabilities and Hospitals.
The Rhode Island state agency which funds services for adults with developmental disabilities has acknowledged for the first time that its underlying reimbursement system for private providers is structurally deficient for complying with the Americans With Disabilities Act as required by a 2014 federal civil rights decree.
While the state Department of Behavioral Healthcare, Developmental Disabilities and Hospitals (BHDDH) has pursued services promoting greater independence for adults with developmental disabilities, “the underlying reimbursement system has lagged,” according to a statement of the scope of work outlined for a consortium tasked with reviewing reimbursement rates.
The rate structure “is grounded in past practices and cost bases associated with the provision of services in the sheltered workshop setting,” BHDDH officials wrote.
“In order to adequately meet consumers’ needs, providers have been paid supplemental funds to address the deficiency in the payment rates,” BHDDH explained in the contract.
BHDDH has a contract with the New England States Consortium Systems Organization (NESCSO) to update a rate structure that has not been reviewed for eight years and to suggest alternates to the current payment methods.
In describing the work ahead for NESCSO, BHDDH says it is:
“seeking to further promote the development of a service system and associated reimbursement arrangements that maximize the opportunity for persons with DD to participate to the fullest possible in community-based activities.”
In 2014 the U.S. Department of Justice found that the reimbursement system incentivized segregated care in sheltered workshops and day centers in violation of the Integration Mandate of the ADA, reinforced by the U.S. Supreme Court in the Olmstead decision.
The Obama administration began vigorously enforcing the Olmstead decision in 2009, but the consent decree in Rhode Island was the first settlement that addressed segregation in daytime services rather than housing.
The consent decree provides a decade-long period of federal oversight of the state’s efforts to change the system. Enforcement of the consent decree entered its sixth year April 9. It will take at least another year for changes in rates and payment methods to go into effect, with the approval of the General Assembly. Enforcement of the decree is set to expire in 2024, but the state would have to show substantial compliance before federal oversight ends.
While some improvements in services have been made, the contract with NESCSO indicates that BHDDH officials believe the reimbursement system has held back compliance efforts.
Staffing Ratios Hinder Needed Flexibility
The underlying problem, said the BHDDH director in an interview, is a rule that requires a ratio of 60 percent funding for community-based activities and 40 percent funding for center-based daytime care in each client’s individual authorization.
The contract language alludes to this situation in describing staffing ratios. It says two areas of “particular focus” are daytime rates paid for employment-related and non-work services. In sheltered settings, for example, there might be one worker for every ten clients. But in the community the number of clients for each worker would have to be much smaller.
Rebecca Boss, the BHDDH director, said the department seeks a “predictable rate structure not driven by very precise ratios” but rather by the needs and preferences of individual clients.
The supplemental payments intended to mitigate the deficiencies in the underlying system “are an increasing portion of overall payments, reflecting the inadequacy of the current rates,” the contract language explained.
According to department officials, that language was meant to refer to the historical trend, in which supplemental payments had increased to as much as $7.8 million in a three-month period.
Boss froze new approvals at the end of 2017, except for emergency health and safety considerations and a couple other narrowly defined exceptions, to try to curb a multi-million dollar deficit at a time when Governor Gina Raimondo seemed inclined to cut developmental disability services significantly.
According to records BHDDH turns in to the General Assembly every month, the supplemental payments from January through March of this year have declined to $3.6 million, about half the total for the same period in 2018.
Historically, supplemental payments have been awarded only when consumers, families, or providers have made successful appeals of individual authorizations. The appeals, which often have required considerable time and energy, must be made annually, or the authorization reverts to the original amount. The appeals process is but one facet of what many families and providers describe as an unstable system.
Kerri Zanchi, director of the Division of Developmental Disabilities, said supplemental payments are still a big part of reimbursements to private providers, and BHDDH wants NESCSO and its consultants to scrutinize them as part of the review process.
Study Commission To Hear from NESCSO
The rate review coincides with the work of a special legislative commission studying the current reimbursement system, called Project Sustainability.
On June 18, the commission will meet to hear presentations about employment and transportation issues from Scott Jensen, director of the Department of Labor and Training; and from Scott Avedesian, CEO of the Rhode Island Public Transit Authority.
On June 25, the executive director of NESCSO, Elena Nicolella, is scheduled to appear before the commission to give an update on the rate review now being conducted by four consultants under NESCSO’s supervision.
In the meantime, some commission members have given BHDDH their own statements on how they think consultants should approach the work and their ideas for a new system of services that allow consumers and their families to shape the way state funds are used.
A spokeswoman for providers has urged NESCSO and its consultants to gain a thorough understanding of what it costs for a private agency to provide services under the terms of recently-revised regulations for provider operations and quality certification standards.
These bureaucratic steps are part of the state’s efforts to comply with the consent decree and the federal Medicaid Home And Community Based Final Rule (HCBS). Like the consent decree, HCBS embraces the integration mandate of the ADA, but it is a nationwide rule applying to all community-based services funded by Medicaid.
Paradox In Unspent Funds For Employment
Tina Spears, executive director of the Community Provider Network of Rhode Island, warned that simply looking at the way providers utilize the current reimbursement model, which is based on segregated care, will not give the complete picture of the needs of the system.
She did not mention specifics, but a case in point is the performance-based supported employment program, which was funded by a $6.8 million allocation made by the General Assembly in the fiscal year that began July 1, 2016. That allocation still has not been completely spent.
Excluding a start-up period from January through June of 2017, the program spent $2.5 million the first year, from July 1, 2017 through June 30, 2018. It’s expected to spend $4 million in the fiscal year ending June 30, according to a BHDDH spokesman.
Providers initially complained that they could not meet their costs with the series of one-time incentives offered by the program, which was built on same reimbursement system designed for center-based care.
Incentives and enhancements were made more generous during the second year, and negotiations are underway for a third year of the program.
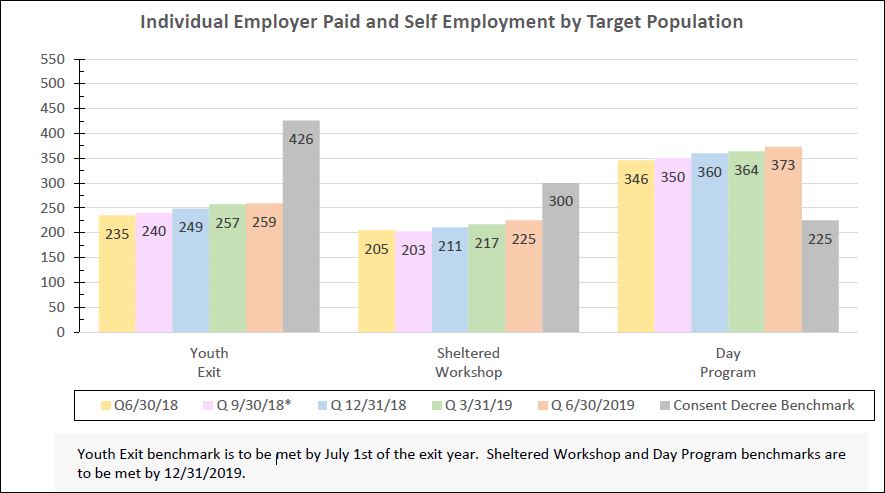
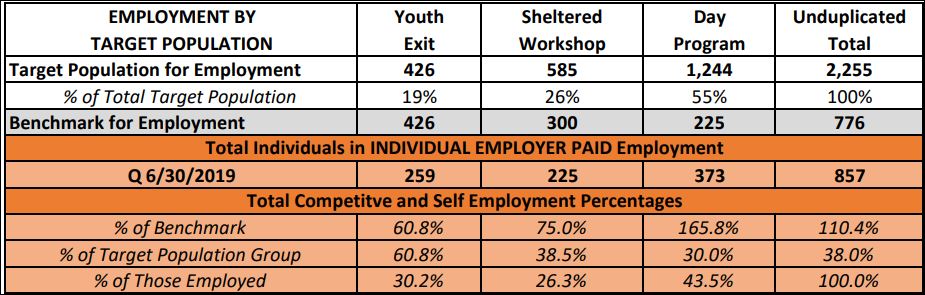
In the meantime, Rhode Island’s last sheltered workshop closed last year and BHDDH says community-based, competitive employment has increased to about 29 percent of adults with developmental disabilities.
A study released by two nationwide associations of providers in January said Rhode Island’s rate of competitive employment was about 19 percent, but that figure dated from 2015. The “Case for Inclusion” ranked Rhode Island 32nd in the nation on its integration efforts. It was compiled by ANCOR - the American Network of Community Options and Resources, and UCP – United Cerebral Palsy.
Consumers Want More Control Over Money Assigned To Them
Kevin Nerney, executive director of the Rhode Island Developmental Disabilities Council, and Kelly Donovan, who receives state-funded supports, each called for a system that allows greater consumer control of state funding and greater flexibility in the way it is used.
The state should “ensure that funding is available across all imaginable living arrangements,” particularly in situations where a consumer owns or rents a property and a caregiver or family would like to move in. The caregiver or consumer should be allowed a stipend, as is permitted in many other states, to make this type of arrangement viable, Nerney said.
The state should also ensure that adults with developmental disabilities have the support of familiar staff while they are hospitalized to avoid the trauma of being in an unfamiliar environment where they can neither make themselves understood nor understand what is being said to them, Nerney said.
In addition, the state should adopt a way to assess the support a person receives from family or friends in deciding funding levels. While most of those receiving services from the Division of Developmental Disabilities live in the family home, that home may include a large healthy family, a single aging parent, or a grandparent with Alzheimer’s and a sibling who also has significant needs for support, Nerney said.
And he called for more funding for those hired by self-directed consumers and their families to write support plans necessary to qualify for state funding. The expectations for the plan writers have multiplied over the last 20 years but the fees remains the same at $500 for the initial plan and $350 for an annual renewal, Nerney said. There should be an allowance for self-directed families who need ongoing coordination of services, he said.
Kelly Donovan, who herself receives services from BHDDH gave a concrete example of what greater control and flexibility might look like.
She said people should be able to enjoy an outing without:
A: going home early because a staffer’s shift ends
B: taking everyone in your group home with you, even if one or more of them really didn’t want to come.
“People should be able to have their designated time to themselves and opportunities to be involved in community activities,” she said.
The public may submit comments or questions about the rate review process by email at BHDDH.AskDD@bhddh.ri.gov. Please copy and paste the email address into your email program, or get a link by visiting http://www.bhddh.ri.gov/developmentaldisabilities/community_forums_event.php
In response to this article, Randal Edgar, a spokesman for BHDDH, released the following statement on June 17:
The article published on June 12 on the Olmstead Updates blog presents a misleading picture of Rhode Island’s system of care for adults with developmental disabilities.
The headline claims this system “promotes segregated care.”
This assertion is false.
The article attempts to back up this assertion up by referring to language in a state contract with a consultant that is reviewing the rates paid to DD providers. But in referencing the contract language, the article misreads the intent of that language.
The contract language speaks from a historical perspective. It states that while the Department of Behavioral Healthcare, Developmental Disabilities and Hospitals has pursued the development of “a services system that supports greater independence” for the DD population, “the underlying reimbursement system has lagged.” It goes on to say that the “basis for the development of prevailing rates is grounded in past practices and cost bases associated with the provision of services in the sheltered workshop setting.”
Acknowledging that the existing rates are grounded in past practices and need to be updated is not the same as saying the system as it operates today promotes segregated care, and in saying it does, the article ignores and/or minimizes many steps the department has taken to improve the care provided to adults with developmental disabilities. It should be noted that the reporter met with BHDDH officials for more than an hour but did not press this assertion and obtain their view of the contract language.
The article is wrong again when it states that department froze new approvals for supplemental payments in 2017 to help offset a budget deficit. The department reduced those approvals, applying more stringent standards, not because of a possible budget deficit but because this made sense from a policy standpoint.
Finally, the article gives voice to people outside the department, asking them to describe where the DD care system should go, without giving BHDDH officials a chance to share their vision. In the process, it conveys a false impression that BHDDH officials are not passionate about moving this system forward.
We are disappointed that the article did not present a more complete and accurate picture.
Separately, the public may submit comments or questions about the rate review process by email at BHDDH.AskDD@bhddh.ri.gov. Please copy and paste the email address into your email program, or get a link by visiting http://www.bhddh.ri.gov/developmentaldisabilities/community_forums_event.php